Introduction
Allergic rhinitis, commonly known as hay fever, is a prevalent allergic condition that affects millions of people worldwide. It occurs when the immune system reacts to allergens, leading to a range of uncomfortable symptoms.
Allergic Rhinitis Definition
It is an IgE-mediated immunologic response of nasal mucosa to airborne allergens and is characterized by watery nasal discharge, nasal obstruction, sneezing and itching in the nose. This may also be associated with symptoms of itching in the eyes, palate and pharynx.
What Is Allergic Rhinitis?
Allergic rhinitis is an allergic reaction that primarily affects the nose and throat. It occurs when the immune system mistakenly identifies harmless substances, such as pollen, dust mites, pet dander, or mold spores, as threats. The immune system responds by releasing chemicals, including histamines, which trigger allergy symptoms.
Types Of Allergic Rhinitis
•Seasonal. Symptoms appear in or around a particular season when the pollens of a particular plant, to which the patient is sensitive, are present in the air.
•Perennial. Symptoms are present throughout the year.
Common Causes of Allergic Rhinitis
- Pollen: Pollen from trees, grasses, and weeds is a common allergen that can trigger seasonal allergic rhinitis, often referred to as “hay fever.” Different plants release pollen at different times of the year, leading to spring, summer, or fall allergies.
- Dust Mites: These microscopic creatures thrive in household dust, bedding, and upholstery. Dust mites can trigger year-round allergic rhinitis.
- Pet Dander: Proteins found in the skin cells, urine, and saliva of pets can cause allergic reactions in sensitive individuals. Cats and dogs are common sources of pet dander allergies.
- Mold Spores: Mold grows in damp environments and releases tiny spores that can become airborne. Mold spore allergies can occur both indoors and outdoors.
- Other Allergens: Allergic rhinitis can also be triggered by allergens like cockroach droppings or specific occupational allergens like chemicals or latex.
Allergic Rhinitis Symptoms
The symptoms of allergic rhinitis can vary in severity and may include:
- Sneezing
- Runny or stuffy nose
- Itchy or watery eyes
- Postnasal drip
- Fatigue
- Coughing
- Sore throat
- Loss of smell or taste (less common)
The cardinal symptoms of seasonal nasal allergy include paroxysmal sneezing, 10–20 sneezes at a time, nasal obstruction, watery nasal discharge and itching in the nose. Itching may also involve eyes, palate or pharynx. Some may get bronchospasm. The duration and severity of symptoms may vary with the season.
Symptoms of perennial allergy are not so severe as that of the seasonal type. They include frequent colds, persistently stuffy nose, loss of sense of smell due to mucosal oedema, postnasal drip, chronic cough and hearing impairment due to eustachian tube blockage or fluid in the middle ear.
These symptoms can significantly impact a person’s quality of life, leading to sleep disturbances, reduced productivity, and discomfort.
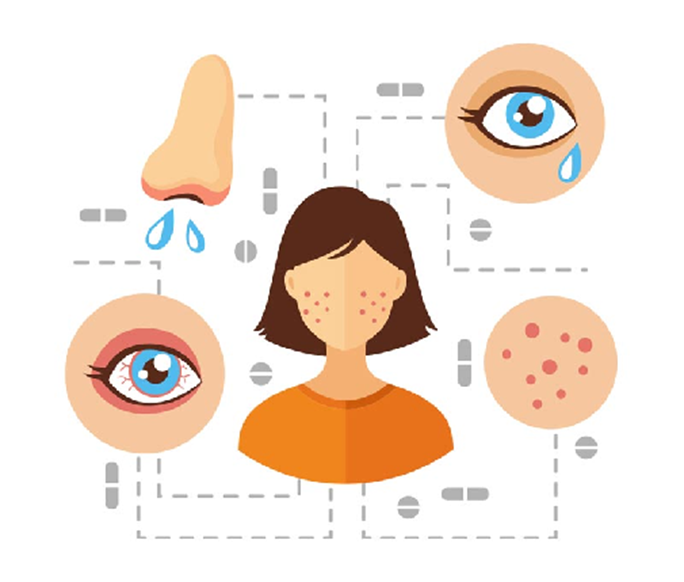
Signs Of Allergic Rhinitis
• Nasal signs: include transverse nasal crease—allergic salute. pale and oedematous nasal mucosa which may appear bluish. Turbinates are swollen. Thin, watery or mucoid discharge is usually present.
•Ocular signs: oedema of lids, congestion and cobblestone appearance of the conjunctiva, and dark circles under the eyes (allergic shiners)
•Otologic signs: include retracted tympanic membrane or serous otitis media as a result of eustachian tube blockage.
•Pharyngeal signs: include granular pharyngitis due to hyperplasia of submucosal lymphoid tissue.
Laryngeal signs: include hoarseness and oedema of the vocal cords.



Tests Or Laboratory Investigations For Allergic Rhinitis
If you suspect you have allergic rhinitis, it’s essential to consult a healthcare provider for a proper diagnosis. Diagnosis typically involves a medical history review, physical examination, and allergy testing, which may include skin prick tests or blood tests.
•Total and differential count. Peripheral eosinophilia may be seen but this is an inconsistent finding.
•Nasal smear. It shows large number of eosinophils in allergic rhinitis.
•Nasal provocation test
•Skin tests. These tests help to identify a specific allergen.
•Skin prick test. A drop of concentrated allergen solution is introduced to the dermis. A positive reaction is manifested by the formation of a central wheal and a surrounding zone of erythema (flare) within 10–15 min.
•Specific IgE measurements
•Radioallergosorbent test (RAST)
Allergic Rhinitis Treatment
- Allergen Avoidance: Identifying and avoiding allergens is an essential part of managing allergic rhinitis. This may involve keeping windows closed during high pollen seasons, using allergen-proof covers for bedding, and regularly cleaning your home to reduce dust mites and mold.
- Drugs for Allergic Rhinitis: Over-the-counter or prescription medications can help relieve symptoms. Antihistamines, decongestants, nasal corticosteroids, and antileukotriene drugs are commonly used to manage allergic rhinitis.
- Antihistamines: To control rhinorrhea, sneezing and nasal itch. May cause drowsiness. E.g. Cetirizine, Loratadine.
- Sympathomimetic drugs: α−agonists constrict blood vessels, reduce congestion and edema, CNS stimulation for drowsiness (pseudoephedrine, phenylephrine)
- Corticosteroids: orally and limited to acute episodes not controlled by other measures.
- Sodium cromoglycate: stabilizes mast cells and prevents degranulation
- Anticholinergics: block rhinorrhea (ipratropium bromide)
- Leukotriene receptor antagonists: Montelukast, zafirlukast
- Anti-IgE: reduces IgE level, anti inflammatory (omalizumab)
- Immunotherapy (Allergy Shots): For individuals with severe allergic rhinitis that doesn’t respond well to other treatments, allergen immunotherapy may be recommended. This involves gradually exposing the individual to increasing amounts of allergens to desensitize their immune system.
- Nasal Irrigation: Saline nasal irrigation with a neti pot or saline nasal sprays can help relieve congestion and reduce the buildup of allergens in the nasal passages.
Conclusion
Allergic rhinitis is a common condition that can cause a range of bothersome symptoms. Understanding its causes and management options is essential for improving your quality of life. If you suspect you have allergic rhinitis, consult a healthcare provider to determine the best course of action. With proper treatment and allergen avoidance, you can effectively manage allergic rhinitis and enjoy a better quality of life, free from the discomfort of allergy symptoms.
